What is Endoscopic Submucosal Dissection (ESD)
14 December, 2022
It is a flexible, tube-like instrument known as an endoscope which is used in the minimally invasive treatment known as Endoscopic Submucosal Dissection (ESD) to remove precancerous and cancerous regions from the Gastro Intestinal (GI) tract. The term "submucosal" refers to the procedure's focus on tumors that are under the GI tract's lining (mucosa). These tumors may be near to muscular tissue and may be challenging to totally remove using normal techniques.
This operation is carried out by gastroenterologists and medical professionals specially expertise to treat the GI system. The doctor will put the endoscope through the mouth for upper GI tumors or through the anus for lower GI tumors depending on where in the GI tract the tumor is placed. Most people recover from ESD as an outpatient surgery and return home the following day. This procedure requires a high precision and accuracy to perform and it is not easily available at any hospital across the country.
Who needs Endoscopic Submucosal Dissection (ESD)?
The following cancers and lesions that affect the submucosa, the region between the lining of internal organs and the muscle wall can be treated with the ESD procedure:
Esophageal Barrett's disease
Cancerous tumors or colon polyps in the early stages, such as colorectal, stomach, or esophageal cancer.
Esophageal, stomach, or colon tumors that have not yet spread to the GI wall's deeper layer.
For the removal of some growths, particularly those without distinct borders or those that are too large to be removed in one piece by conventional procedures, ESD may be a more effective choice than endoscopic mucosal resection (EMR). In these situations, ESD can reduce the danger of the tumor spreading.
In order to provide better therapy, ESD can also assist the doctor in staging the GI cancer (by identifying its spread).
How is Endoscopic Submucosal Dissection (ESD) done?
It is usually done by the gastroenterologist. Before the surgery, the patient is supposed to:
1. Follow a liquid diet and a laxative or enema to clear the bowels before a lower GI tract operation.
2. Avoid eating or drinking for 12 hours before an upper GI tract surgery to ensure that the food pipe or esophagus is clean of food.
3. In case of any allergies, the doctor suggests the required medicines.
4. The patient is sedated to make him/her asleep during the procedure so that the patient does not experience any pain.
5. Depending on where the tumor is, a high-definition endoscope is inserted through the mouth or anus.
6. The entire procedure is performed while viewing it on a screen to prevent any damage to the nearby tissue.
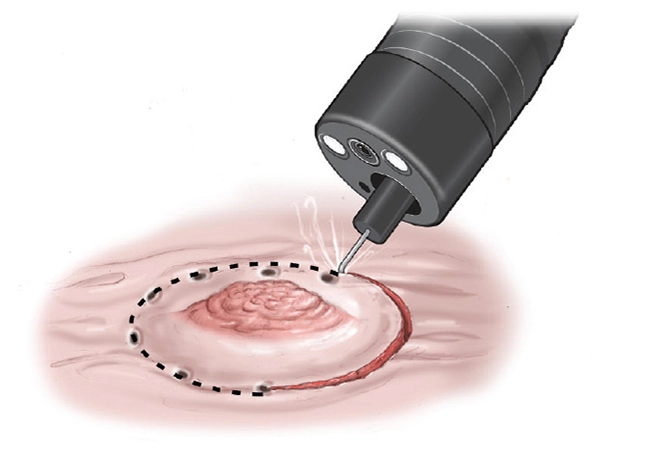
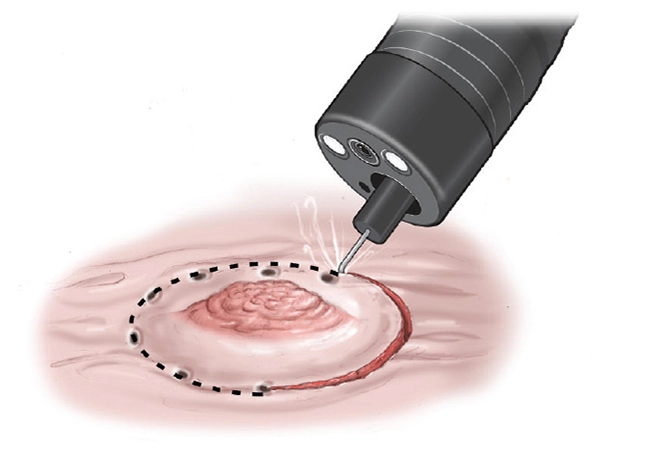
7. With the use of a specific tool inserted through the endoscope tube, the tumor is located and its boundaries.
8. To detach the tumor or lesion from the muscle wall, a solution is injected beneath it. By doing this, the procedure's potential for damaging nearby tissue is also reduced.
9. Using a high-frequency electrical current with the help of an electrosurgical knife the tumor tissue is "cut" free from the GI wall and the blood vessels are sealed by the electrical current which lessens the bleeding.
10. Through the use of an endoscope the removed tissue from the body is then sent to a lab for pathology analysis.
11. Following the ESD operation, the patient's condition is watched over while the sedative wears off. The doctor will then go through the ESD results.
12. The pathologist can determine whether the procedure successfully removed the tumor by examining the tissue samples under a microscope.
13. As the patient heals, he/she might go through sore throat as the endoscope was inserted through your mouth, might have nausea or vomiting if the stomach or intestines were treated and sometimes might face excessive gas, bloating, or pain, particularly if the abdomen was inflated with air during the therapy.